Day :
- Retina & Retinal Disorders|Corneal Diseases

Chair
Ronni M Lieberman
New York City Health and Hospitals Corporation, USA
Session Introduction
Ronni M Lieberman
New York City Health and Hospitals Corporation
Title: Long-term follow-up of intravitreal bevacizumab for the treatment of pediatric retinal and choroidal diseases
Time : 11:55-12:20

Biography:
Abstract:
Cristina Nitulescu
National Institute for Mother and Child Health, Romania
Title: Retinopathy of prematurity in Romania
Time : 12:20-12:45
Biography:
Abstract:
Ashutosh Patel
S.S. institute of Medical Sciences & Research Centre SSIMS & RC, India
Title: Retinopathy of prematurity incidence, risk factors and treatment modalities among premature infants at various neonatal intensive care units of central Karnataka in South India
Time : 12:45-13:10
Biography:
Abstract:

Biography:
Abstract:
Elias F Jarade
Beirut Eye Specialist Hospital, Lebanon
Title: Combined dermoid cyst excision and DALK procedure in 3 years old boy: Split and patch technique for corneoscleral patching
Time : 14:10-14:35

Biography:
Abstract:
- Pediatric Ophthalmology & Research | Pediatric Optometry

Chair
Bruce H Koffler
Koffler Vision Group, USA
Session Introduction
Danielle M Ledoux
Boston Children’s Hospital - Harvard University, USA
Title: Surgical esotropia in Down syndrome patients
Time : 10:30-11:10

Biography:
Abstract:
Bruce H Koffler
Koffler Vision Group, USA
Title: Myopia control in children utilizing gas permeable orthokeratology molding overnight lenses
Time : 15:00-15:25

Biography:
Abstract:
Anna Laura Giacomin
Camposampiero Hospital, Italy
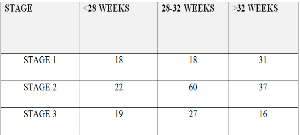
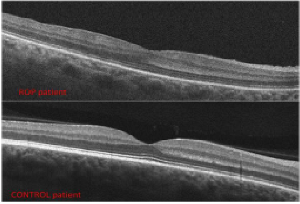
Title: Arrested foveal development and low visual function in babies with history of retinopathy of prematurity
Time : 15:25-15:50

Biography:
Anna Laura Giacomin has completed her Medical degree in 1986 at the Padua University. She has joined as the Ophthalmological Specialist at the Padua University in 1991. In 1996, she joined in the Ophthalmology Unit of the Camposampiero PD Civil Hospital, responsible for the Ophthalmoplastic Service. She has obtained Homeopathy clinic course and in 2011, Master 2° level in Ophthalmoplastic Surgery from Naples Federico II University. From 2005, she is a full Member of the European Society of Ophthalmic Plastic and Reconstructive Surgery.
Abstract:
Lelio Sabetti
University of L’Aquila, Italy
Title: Revital Vision treatment in patients affected by nystagmus
Time : 16:10-16:35
Biography:
Abstract:
Angela Malik
Sidra Medical and Research Center, Qatar
Title: Pediatric contact lens fittings: little eyes big challenges
Time : 16:35-17:00
Biography:
Abstract:
Darakshanda Khurram
Moorfields Eye Hospital Dubai, UAE
Title: Clinical outcomes of surgical management of subluxated lenses in children
Time : 17:00-17:25
Biography:
Abstract:
Biography:
Abstract:
Biography:
Abstract:
- Refractive Errors and Management | Pediatric Neuro-Ophthalmology | Ophthalmology Surgery

Chair
Mikhail G Kataev,
Fyodorov Eye Microsurgery Complex, Russia
Session Introduction
Pedro Mattar
King Khaled Eye Specialist Hospital, Saudi Arabia
Title: Surgical management of ocular motor nerve palsies
Time : 11:30-11:55

Biography:
Abstract:
Serap Azizoglu
Deakin University, Australia
Title: Effects of socioeconomic status on oculo-visual disorders in school children
Time : 11:55-12:20
Biography:
Abstract:
Mikhail G Kataev
Fyodorov Eye Microsurgery Complex, Russia
Title: Oculoplasty for saving vision in children
Time : 12:20-12:45

Biography:
Abstract:
Ayad Shafiq
Newcastle Eye Centre, UK
Title: Contralateral effect of micro-dose bevacizumab (Avastin) injection in zone 1 aggressive posterior retinopathy of prematurity (APROP)
Time : 12:45-13:10
Biography:
Abstract:
Elias F Jarade
Beirut Eye Specialist Hospital, Lebanon
Title: Pediatric keratoconus in a tertiary referral center: Incidence, presentation, risk factors, and treatment
Time : 13:45-14:10

Biography:
Abstract:
Lelio Sabetti
University of L’Aquila, Italy
Title: Choline in association with Bangerter filters for the treatment of amblyopia
Biography:
Abstract:
Antonella Vecchies
University of Padua, Italy
Title: Management of scleral lenses in pediatric age
Time : 14:35-15:00
Biography:
Abstract:
Andrea Binotto
Camposampiero Hospital, Italy
Title: Poor oculomotor- visual skills efficiency correlates with dyslexia and low reading performance
Time : 15:00-15:25
Biography:
Abstract:
Biography:
Abstract:
Elias F. Jarade
Beirut Eye Specialist Hospital, Lebanon
Title: Safety and efficacy of sequential intracorneal ring segment implantation and crosslinking in pediatric keratoconus
Time : 16:10-16:35

Biography:
Abstract:
Goshevska Dashtevska Emilija
University Eye Clinic, Macedonia