Day 1 :
Keynote Forum
Prof. Farhad Hafezi
ELZA Institute, Switzerland
Keynote: The Window into their future: Screening & Early Detection of Corneal Diseases in Pediatric Patients
Time : 10:05-10:35

Biography:
Abstract:
- Retina & Retinal Disorders|Corneal Diseases

Chair
Ronni M Lieberman
New York City Health and Hospitals Corporation, USA
Session Introduction
Ronni M Lieberman
New York City Health and Hospitals Corporation
Title: Long-term follow-up of intravitreal bevacizumab for the treatment of pediatric retinal and choroidal diseases
Time : 11:55-12:20

Biography:
Abstract:
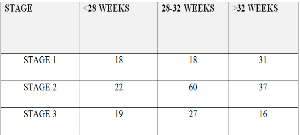
Cristina Nitulescu
National Institute for Mother and Child Health, Romania
Title: Retinopathy of prematurity in Romania
Time : 12:20-12:45
Biography:
Abstract:
Ashutosh Patel
S.S. institute of Medical Sciences & Research Centre SSIMS & RC, India
Title: Retinopathy of prematurity incidence, risk factors and treatment modalities among premature infants at various neonatal intensive care units of central Karnataka in South India
Time : 12:45-13:10
Biography:
Abstract:

Biography:
Abstract:
Elias F Jarade
Beirut Eye Specialist Hospital, Lebanon
Title: Combined dermoid cyst excision and DALK procedure in 3 years old boy: Split and patch technique for corneoscleral patching
Time : 14:10-14:35

Biography:
Abstract:
- Pediatric Ophthalmology & Research | Pediatric Optometry

Chair
Bruce H Koffler
Koffler Vision Group, USA
Session Introduction
Danielle M Ledoux
Boston Children’s Hospital - Harvard University, USA
Title: Surgical esotropia in Down syndrome patients
Time : 10:30-11:10

Biography:
Abstract:
Bruce H Koffler
Koffler Vision Group, USA
Title: Myopia control in children utilizing gas permeable orthokeratology molding overnight lenses
Time : 15:00-15:25

Biography:
Abstract:
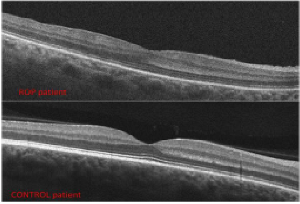
Anna Laura Giacomin
Camposampiero Hospital, Italy
Title: Arrested foveal development and low visual function in babies with history of retinopathy of prematurity
Time : 15:25-15:50

Biography:
Anna Laura Giacomin has completed her Medical degree in 1986 at the Padua University. She has joined as the Ophthalmological Specialist at the Padua University in 1991. In 1996, she joined in the Ophthalmology Unit of the Camposampiero PD Civil Hospital, responsible for the Ophthalmoplastic Service. She has obtained Homeopathy clinic course and in 2011, Master 2° level in Ophthalmoplastic Surgery from Naples Federico II University. From 2005, she is a full Member of the European Society of Ophthalmic Plastic and Reconstructive Surgery.
Abstract:
Lelio Sabetti
University of L’Aquila, Italy
Title: Revital Vision treatment in patients affected by nystagmus
Time : 16:10-16:35
Biography:
Abstract:
Angela Malik
Sidra Medical and Research Center, Qatar
Title: Pediatric contact lens fittings: little eyes big challenges
Time : 16:35-17:00
Biography:
Abstract:
Darakshanda Khurram
Moorfields Eye Hospital Dubai, UAE
Title: Clinical outcomes of surgical management of subluxated lenses in children
Time : 17:00-17:25